The Power of Prevention: Meet the Turning the Tide Violence Intervention Program

5.30.2024
Turning the Tide Violence Intervention Program (TTVIP) is a Charleston-based hospital-based violence intervention program (HVIP) working to improve health and quality of life outcomes for youth and young adult victims community violence that are treated at MUSC Health’s Level 1 adult and pediatric trauma centers.
As the Program Director of the TTVIP, I manage the day-to-day operations of program implementation. My background is in public health, and I have always valued the power of prevention. Working in the injury prevention field showed me the disparities of community gun violence. Over the years, I educated myself on the preventability of this public health issue and its disparate impact on communities. The injustice that two kids growing up in zip codes right next to each other could have such profoundly different childhoods—one with frequent exposure to gun violence, and one blissfully ignorant to it—was unsettling. I was working at a trauma center at the time, so addressing the impact of violence through the hospital violence intervention program (HVIP) model made perfect sense to me.
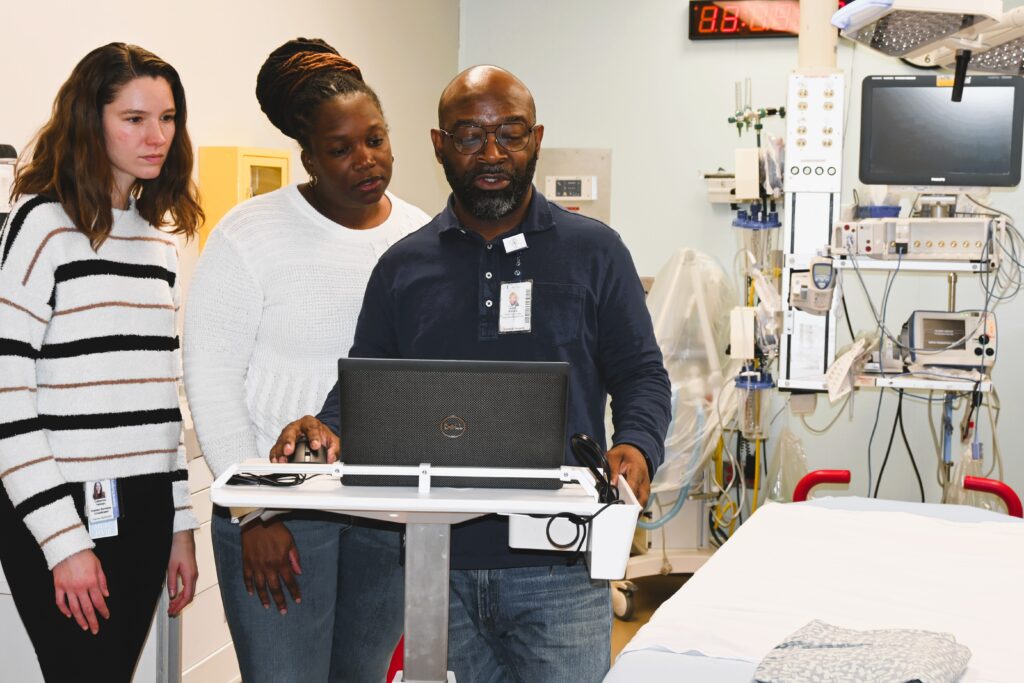
No two days are ever the same in our line of work. I work alongside three full-time violence intervention client advocates, who work on-call 24/7 to ensure support for patients and families whenever needed. For the on-call advocate, their day typically involves responding to the trauma bay for newly injured patients being treated at our trauma center, making bedside visits to patients who are still hospitalized, and liaising with the clinical care team.
Time at the bedsides of violently injured patients and their families is a critical opportunity for intervention. This practice is the cornerstone of hospital-based violence intervention programs (HVIPs). TTVIP’s client advocates are trained in:
- Crisis management,
- Trauma-informed care, and
- Anti-retaliation counseling.
All of these skills are employed during a patient’s hospitalization following a violent injury. During this time, the client advocate is:
- Building rapport with the patient,
- Assessing their eligibility for long-term wraparound services, and
- Preparing a safety plan for discharge.
All TTVIP services are voluntary. If a patient consents, client advocates who worked with hospitalized patients will follow up with them following their discharge.

More about our client advocates:
-
Over time, client advocates work to empower and educate their patients/families to meet their needs and goals independently.
Client advocates perform a comprehensive needs and risk assessment. This assessment obtains a baseline history of a patient’s psychosocial needs. It also identifies modifiable risk factors contributing to their community violence exposure.
Client advocates use a patient-centered approach. They use motivational interviewing techniques to create brief action plans with patients. These plans identify healthcare- and community-based services and resources. Access to these resources may:
- Improve patients’ injury recovery,
- Address their socioeconomic needs, and
- Improve their quality of life outcomes.
Over time, client advocates work to empower and educate their patients/families to meet their needs and goals independently.
On average, patients receive intervention services for 6–12 months after injury — depending on the extent of their needs. These intervention services may include mentorship and/or peer counseling, and transportation assistance. Advocates also extend warm referrals to local services and resources for:
- Education,
- Substance use,
- Employment,
- Mental health care,
- Housing, and more.
Our client advocates meet our patients where they’re comfortable: in their homes, schools, and in their communities. Our client advocates also document their work at each intervention step to help support case management, program evaluation, quality improvement activities, and grant writing and reporting.

In 2022, TTVIP received a grant from the Everytown Community Safety Fund (CSF). This funding has provided salary support to one of our client advocates for the last two years, which has been critical in sustaining our frontline team. The ripple effects of this funding support have been invaluable for us. In addition to providing much-needed job security in the short term, the funding allowed us to hire an additional client advocate. This addition was necessary to meet the needs of our patient volume and has reduced caseloads to a more manageable and effective level.
More about caseload size
-
A manageable caseload improves the quality and effectiveness of the intervention with each patient.
Caseloads are the number of clients assigned to each advocate or provider. Client advocates average a caseload of approximately 15 patients at a time. Sustainable caseloads positively impact the quality of intervention each patient and family receives. Manageable caseloads also prevent provider burnout in multiple ways. Advocates can experience moral distress when they don’t have enough time to assist each patient. Reduced caseload sizes allow advocates to have enough resources to support each patient and family. Finally, at TTVIP, we have someone on call 24/7. With CSF funding support, each client advocate spends less time on call which contributes to more manageable caseloads and prevents burnout.
The CSF has professionally and programmatically supported TTVIP. The CSF hosts a quarterly call that offers a platform for more informal support among fellow grantees. Other CSF offerings that have added immense value to our program include:
- Stipends to attend the Cities United Annual Conference
- Various training by experts in the violence intervention field
- Opportunities to uplift and amplify the work of our program, including a presentation at the RISE Summit.
These activities are beneficial to a younger program like TTVIP. They ensure and affirm that we’re following best practices for our patients, families, frontline workers, and community partners.
HVIPs interrupt the cycle of violence by intervening with some of those at the highest risk of experiencing gun violence: victims. Once violently injured, victims are at even higher risk of experiencing another violent injury. TTVIP uses the public health approach to prevent future violence. We do so by promoting protective factors and mitigating risk factors that influence a person’s repeat exposure to gun violence. By addressing our patients’ psychosocial needs, we can effectively reduce their risk of re-victimization and improve both their injury outcomes and quality of life. In other words, we’re the epitome of “preserving and optimizing human life”: The mission of MUSC.
TTVIP was the first, and is currently the only, HVIP in South Carolina. The HVIP model is nationally growing in popularity. However, HVIPs are only being implemented in a relatively small portion of trauma centers in the U.S. In the South, HVIPs also face unique implementation challenges. One challenge is a larger “catchment area,” or the geographical area served by a hospital. Southern HVIPs can contain places with varying levels of population density, from urban centers to deeply rural areas. The varied catchment area size creates challenges for the availability of and proximity to:
- Resources and services,
- In-person case management, and
- Transportation.
HVIP work has a significant impact on healthcare providers who are also on the frontlines of the gun violence epidemic. These providers bear witness to the devastating physical, psychological, interpersonal, and financial consequences of community violence, which can be deeply traumatic. At TTVIP, we try to practice what we preach to our patients and families by prioritizing our own mental health and well-being. This looks different for each team member, however, as a group, we:
- Participate in resiliency sessions with a therapist on staff at MUSC;
- Promote using sick leave and PTO to care for ourselves and our families;
- Utilize flexible work schedules;
- Offer to staff cases that need additional support; and
- Offer opportunities to network with other frontline workers who understand this work—including vicarious trauma and burnout challenges—best.
Increasing investment in community violence intervention work would reduce much of the undue physical and emotional burden placed on our frontline workers. We need more research to understand how HVIPs contribute to preventing burnout in healthcare providers. At TTVIP, however, we have anecdotally seen a positive impact. Barely six months after TTVIP launched, a pediatric emergency department nurse shared that she sleeps better at night knowing that her patients are going home with more support and resources than before.
Mental Health Awareness Month and TTVIP
-
We recently hired our first mental health clinician, who joined our team the first week of May.
This Mental Health Awareness Month, marked in May, is particularly special to TTVIP. We recently hired our first mental health clinician, who joined our team the first week of May. This clinician will be dedicated to TTVIP’s patients and families. The clinician will offer:
- Bedside introductions and coping strategy education sessions during hospitalization,
- PTSD and depression screenings at 30 days post-injury, and
- Longer-term treatment plans as needed.
We pursued grant funding to support this role in response to our frontline workers’ ongoing experiences. Advocates were trying to connect their patients and families to mental health services. However, it was challenging for people to access these services due to long wait list periods or out-of-pocket expenses. This new mental health clinician will work with our client advocates to address these issues and “co-treat” patients and families. The client advocate will work to address a patient’s socioeconomic needs (which often create barriers to care). At the same time, the mental health clinician can treat their mental health needs with a culturally competent, trauma-focused approach. We’re thrilled to close the gap on this critical service need for our community.
Mental health is a critical healthcare service for victims of violent injury. Victims often exhibit higher rates of PTSD and depression compared to those with other traumatic injuries. Research shows that victims of violence who receive mental health treatment after injury have lower rates of violent injury in the future compared to those who don’t get treatment. Some barriers to accessing mental health treatment can include:
- Personal, community, and social stigma;
- Lack of affordability; and
- A shortage of therapists—particularly BIPOC therapists.
There is still a lot of stigma around mental health treatment in communities of color, particularly for males. Black men experience disproportionately high rates of PTSD and depression after injury. Survivors can exhibit risky behaviors, including:
- Substance misuse,
- Firearm carrying, and
- Gang or group affiliation.
These behaviors may be coping mechanisms for untreated mental health symptoms such as:
- Hypervigilance,
- Trouble sleeping,
- Avoidance,
- Depression, and
- Anger or irritability.
A trauma-informed victim care approach can get to the root of why a person is engaging in these behaviors, which are often survival strategies employed by victims of violent injury to maintain a sense of safety. Addressing the causes of these behaviors can lead to improved health and psychosocial outcomes.
Importantly, there is a false narrative about the correlation between mental illness and the perpetration of gun violence. The reality is that those who suffer from mental illness are more likely to be victims, not perpetrators, of gun violence. Our client advocates serve as credible messengers in our communities and work to address this stigma. They work to normalize symptoms our patients might be experiencing after injury and can encourage seeking treatment.
There are many misconceptions about community violence intervention and gun violence prevention work. TTVIP wants to emphasize that gun violence is a public health issue that requires a public health solution. Community violence disproportionately impacts Black and brown communities due to decades of systematic marginalization. Intervening and preventing future community violence is a strategy that results in more equitable health outcomes for all communities—particularly those who are most impacted.